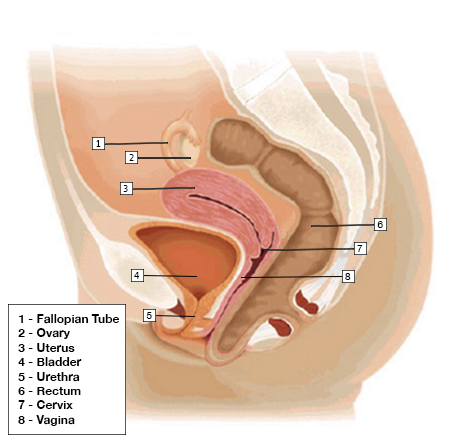
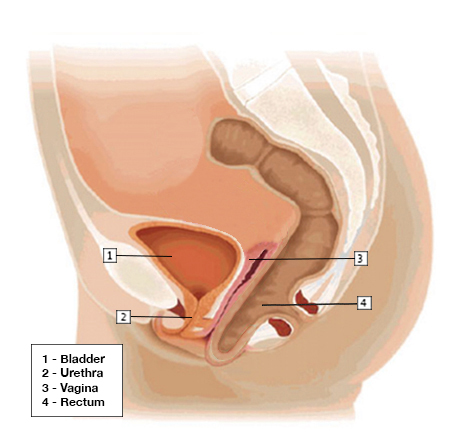
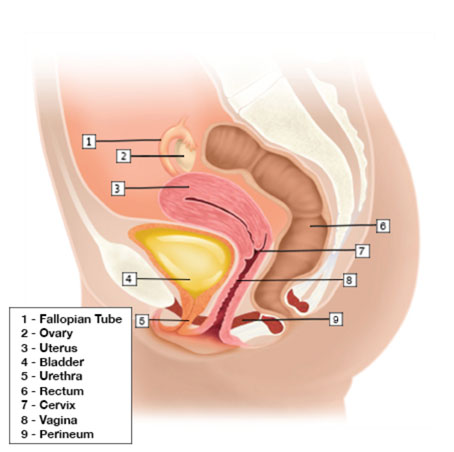
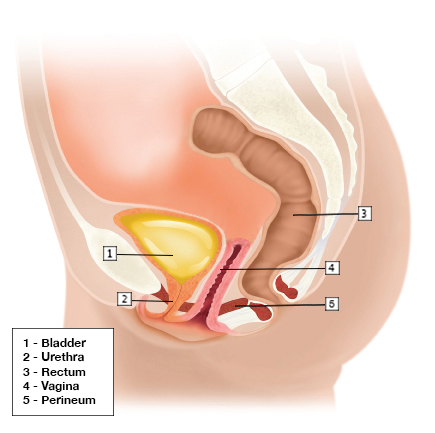
Rectocele is a type of pelvic organ prolapse. Prolapse refers to the dropping of an organ out of its anatomic position. Pelvic prolapses occur when the pelvic muscles and tissues weaken allowing the bladder, rectum, uterus, or small intestine to drop into the vagina. A rectocele occurs when the wall between a woman’s rectum and her vagina weakens allowing the rectum to drop into the vagina.
Rectocele
Book An Appointment
I have nothing but positive things to say about Dr. Shashoua and his entire staff. From day 1, I was treated with nothing but kindness from the front office to the back. My condition was rather complex in that I needed Cystocele, Rectocele and Uterine Prolaspe Repair. My treatments included a Hysterectomy, Da Vinci Sacrocolpoperineopexy and a Mid-Urethral Sling. I had no major issues post-surgery. My pain was managed very well by both Sarah and Kristin. Any issues I had were quickly addressed. Marissa was also a delight. I have 5 kids and Dr. Shashoua very delicately mentioned the need for a hysterectomy. From that moment I knew he was very caring and sensitive to his patients needs. My entire experience was handled with ease, a high level of professionalism and an awesome spirit of providing quality care. I'm so very grateful I chose Austin Urogynecology.
-Tracy G.
A rectocele may be asymptomatic in some women. In others, it may cause the following symptoms:
- A soft bulge of tissue in the vagina that protrudes through the vaginal opening
- Difficulty having a bowel movement
- The need to press your fingers on the bulge in your vagina to help push stool out during a bowel movement
- Sensation of rectal pressure or fullness
- A feeling that the rectum has not completely emptied after a bowel movement
The main factors that contribute to the development of a rectocele are:
- Hereditary factors. Rectoceles tend to run in families. There are genes that code for the supporting structures of the pelvic floor and variations in these genes can lead to weakening of the pelvic floor, allowing for formation of the rectocele.
- Childbirth. Vaginal birth can stretch and weaken the supporting structures of the pelvic floor.v
- Age. As supporting structures of the pelvic floor age, they weaken.
- Chronic constipation and chronic straining during bowel movements.
Perineal descent is often present in women with a rectocele, especially when there is a history of chronic straining from constipation. Some women with perineal descent will push up (splint) their perineum to help evacuate stool during a bowel movement. In addition, women with a rectocele may also have perineal relaxation (stretching and relaxation of the vaginal opening) or fecal incontinence.
Early stage or small rectoceles may be asymptomatic and may not require treatment. A non-surgical treatment for a symptomatic rectocele is a pessary. A pessary is a supportive device inserted into the vagina to reduce or elevate the prolapse. A pessary is typically used in women who are not candidates for surgery due to advanced age or poor health or who prefer not to undergo surgery. A pessary can limit intercourse and therefore may not be a good option for sexually active women who are able to tolerate surgery. Symptoms from a rectocele can improve with pelvic floor exercises or pelvic floor physical therapy. These therapies may slow the progression of the rectocele, but they do no reduce the size of the rectocele.
Surgery to treat a rectocele is elective and is done to relieve symptoms and restore the anatomy of the vagina. The type of surgery recommended, either vaginal or robotic, is based on each individual’s symptoms and exam findings.
Got questions? Need an appointment? We’re here to help!